My PrEP Experience is pleased to launch a new informational resource called "Truvada Track - monitoring insurance and Medicaid coverage of Truvada for PrEP."
This page - accessible via tab at the top of this blog - monitors insurance and Medicaid coverage of Truvada as PrEP . It will be updated frequently. The most current update is always at the top. If you have information about insurance of Medicaid coverage of Truvada for PrEP - including pre-authorization requirements or denials - please share this information with us by sending an email to myprepexperience@gmail.com.
Here is our first update.
• United Healthcare (commercial insurance): Prior authorization required, consistent with indication on label, triggered when Truvada is prescribed without a third agent or in the absence of code for HIV infection (see pictures above)
Questions, concerns, or clarifications - send email to myprepexperience@gmail.com
Here is our first update.
July 1, 2013 update
 |
| Letter from United Healthcare regarding pre-authorization requirements for Truvada as PrEP. |
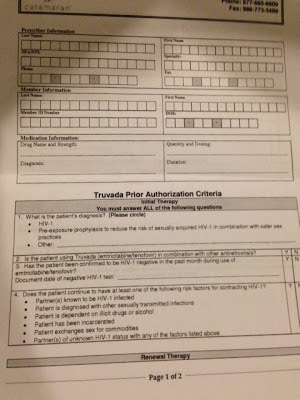 |
| Pre-authorization requirements for Truvada as PrEP from United Healthcare. |
• Aetna (commercial insurance): Prior authorization required, consistent with indication on label, triggered when Truvada is prescribed without a third agent or in the absence of code for HIV infection
• Florida Medicaid: Prior authorization required, consistent with indication on label, triggered when Truvada is prescribed without a third agent or in the absence of code for HIV infection
• New York Medicaid: Prior authorization requires documented HIV- test result; triggered when Truvada is prescribed without a third agent or in the absence of code for HIV infection
• Catamaran (pharmacy benefit management – select clients only): As of 6/25/13 – reports from health care providers of prior authorization impacting new starts on Truvada to confirm diagnosis (treatment vs. PrEP). Appears to allow PrEP use when consistent with label.
Notes:
- Up to July 1, we have not heard of denials of coverage. But pre-authorization requirements, many of which are just starting on July 1, could potentially lead to denial of coverage for Truvada as PrEP.
- "Without a third agent" - Truvada is a combination of 2 drugs, and appropriate treatment for people living with HIV consists of 3 or more drugs. So, when Truvada is prescribed and a third "agent" is not, this signals that Truvada is being prescribed as PrEP.
- United Healthcare is the largest insurer in the U.S., and we understand that approximately 300 of their members (out of a total in the millions) are currently taking Truvada without a third agent. A very, very small percentage of HIV-negative people for whom they provide insurance.
Questions, concerns, or clarifications - send email to myprepexperience@gmail.com
Tidak ada komentar:
Posting Komentar